Patient history
Sophie, a 72 year old lady from Victoria, was diagnosed with oral lichen planus in her forties. Sophie’s condition was reviewed regularly over the following 22 years, at least annually and sometimes more often. Her oral medicine specialist had no concerns. However, five years ago the appearance of her tongue changed.
Initially, Sophie had asymptomatic bilateral striae on her buccal mucosa in a reticular pattern. Biopsy supported the clinical diagnosis. Sophie subsequently developed areas of erythema and ulceration that came and went over a 22 year period. These episodes were irregular, occurring multiple times in some years and other years not presenting at all. They were often associated with stressful periods of her life. Each episode was successfully managed with topical steroids, used sparingly for a short period.
Clinical appearance at presentation
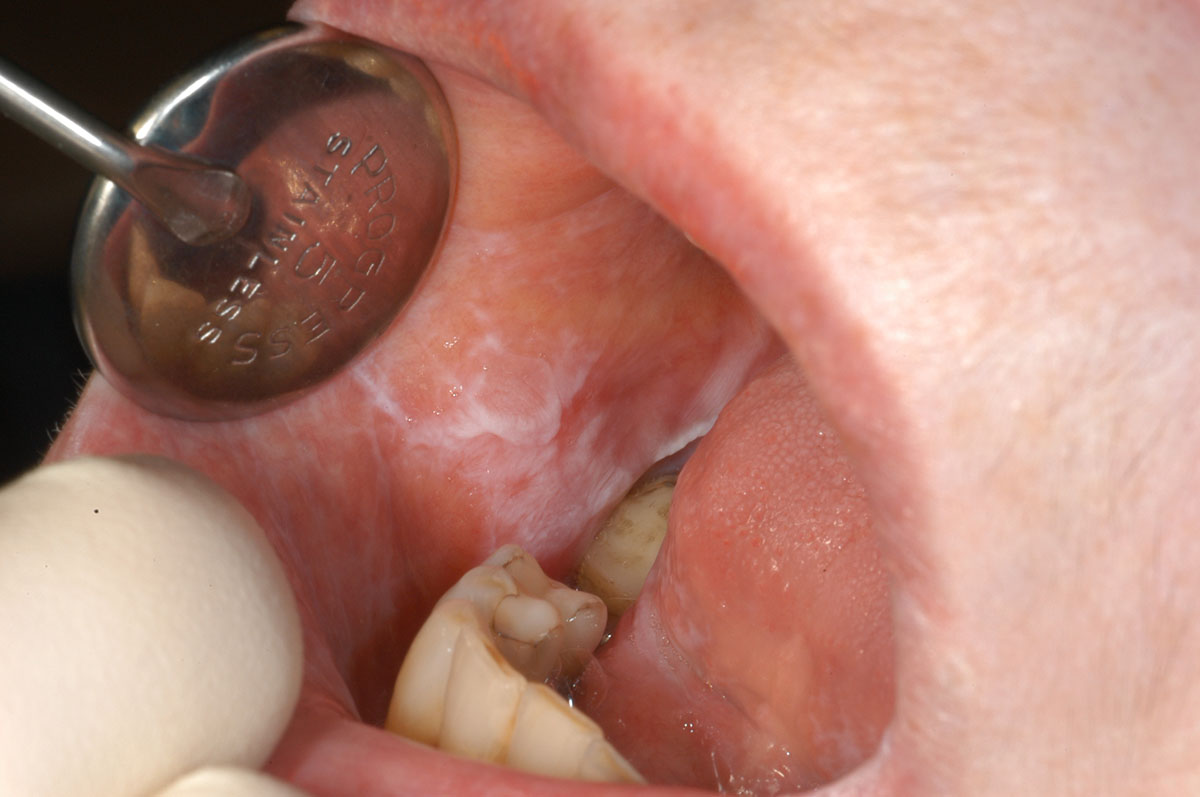
72 year old with reticular oral lichen planus of both left and right buccal mucosa.
Change in clinical appearance
During an oral mucosal review, the dorsal surface of Sophie’s tongue was observed to have thickened, become slightly exophytic and firmer to palpate. An incisional biopsy showed this to be a squamous cell carcinoma. Sophie was referred to The Royal Melbourne Hospital’s head and neck tumour multidisciplinary clinic for definitive treatment, where her tumour was staged as a T1N0M0 (stage I oral cancer).

Patient treatment and outcome
Sophie’s tumour was successfully removed through surgery. She did not require further surgery or treatment. Sophie benefited from supportive rehabilitation with a speech pathologist. She continues to have occasional pain caused by oral lichen planus in other areas of her oral mucosa. Positively, Sophie remains in remission.
Key learning from this case study
- Examination of the oral mucosa is a mandatory part of oral examination, with the potential to prevent or detect oral cancer earlier.
- Patients with oral lichen planus require regular, long-term monitoring for changes in appearance.
- Early diagnosis of oral cancer can lead to excellent prognosis for the patient: with excellent cure rates following minor surgery, minimal functional impairment and few or no aftereffects.
This case study is based on a real case report. Names and identifying details have been changed to protect the privacy of individuals. It was written by Michael McCullough, Professor of Oral Medicine at University of Melbourne Dental School.
