Oral squamous cell carcinoma (oral cancer) can appear as a persisting deep ulceration, a flat or slightly raised lesion, an exophytic papillary or verrucous growth. It is often firm to palpation, and rapidly changes. Oral squamous cell carcinomas are often completely asymptomatic in the initial stages, meaning patients do not present until late – resulting in increased morbidity and mortality. Lesions that persist for longer than two weeks require urgent referral for definitive diagnosis.

A thickened exophytic lump on the left dorsal surface of the tongue that had been increasing in size over the previous six to eight weeks. Female patient with long standing oral lichen planus. Biopsy showed this to be a squamous cell carcinoma.

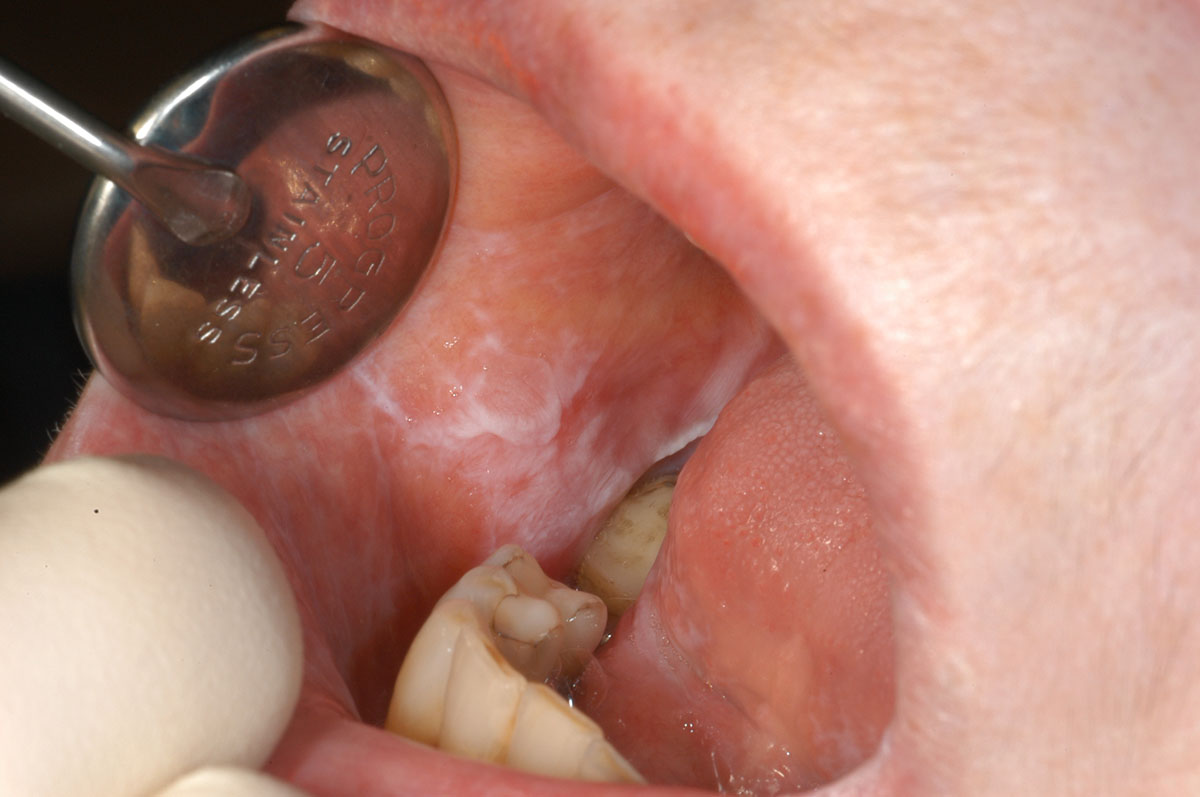
A painful ulcer worsening over a six month period in the posterior right cheek that was painful and very firm to touch. Biopsy showed this to be an invasive squamous cell carcinoma.
Homogenous leukoplakia
Non-homogenous leukoplakia
Verrucous leukoplakia
Nodular leukoplakia
Erythroleukoplakia
Leukoplakia are white plaques that are not caused by any other condition and which have an increased potential for malignant transformation. This is the most common potentially malignant oral mucosal condition.
Potential for malignancy has been reported to be around 1-7% for homogenous leukoplakia, and 5-50% for non-homogenous leukoplakia. While the cause is unknown, risk factors include smoking, drinking alcohol and betel quid chewing.
Diagnosis includes a biopsy for assessment of the presence of dysplasia. Management involves reducing behavioural risks, e.g. cessation of smoking and alcohol. Depending on clinical and histopathological appearance, treatment may involve excision and will require long-term monitoring of all oral mucosa.

A flat homogeneous white plaque present on the ventral surface of the left tongue, extending onto the floor of mouth. This lesion was asymptomatic and only observed on routine examination in a heavy smoker.
Reticular oral lichen planus
Erythematous oral lichen planus
Ulcerative oral lichen planus
Plaque-like oral lichen planus
A chronic, immune-mediated mucosal condition occurring in less than 1% of the population, and more often in middle age and older. Oral lichen planus has a variable clinical appearance with a reticular pattern, the most common consisting of striae bilateral buccal mucosa that can extend to the lateral margins of the tongue. It can also appear as areas of erythema, ulceration and plaque-like regions, or a combination of all of these.
Similar appearance can be observed with drug-associated hypersensitivity reactions, contact hypersensitivity to restorative materials and graft versus host disease.
Symptomatic treatment requires topical anti-inflammatory agents, while asymptomatic lesions require no treatment. Long-term monitoring is advisable as there is a potential for around 1% to undergo malignant transformation.
White striae extending across the right buccal mucosa in a reticular pattern with very little erythema and no ulceration.

White striae extending across the left buccal mucosa in a reticular pattern with very little erythema and no ulceration. This is the same patient as in image above, who presented with bilateral buccal mucosal asymptomatic oral lichen planus.

Striae extending to the depth of the mandibular sulcus on the right buccal mucosa and posteriorly onto the tissue overlying the erupting third molar. This patient’s symptoms were associated with the erupting third molar, not lichen planus.

Striae on the right lateral margin of the tongue with no erythema or ulceration in the same patient as in image above.

An area of striae with erythema and ulceration on the left lateral margin of the tongue in the same patient as in image above. This ulcerated area had been present for several months and was painful to touch. Biopsy of the non-ulcerated region on this site was diagnostic of oral lichen planus.

Extensive ulceration, erythema and striae on the right buccal mucosa that was very painful.

Painful ulceration with erythema and surrounding striae on the right buccal mucosa. This is the same patient as in image above. Extensive mucosal changes were diagnosed as histopathological as oral lichen planus.
Erythema migrans
Geographic tongue
Chronic inflammatory condition of the tongue. Filiform papillae (responsible for giving the tongue its texture and the sensation of touch) on the dorsal surface of the tongue are lost then return, in a recurring pattern across different areas. These patterned areas on the tongue are slightly depressed and red, with a surrounding white rim – giving the appearance of a topographical map, with changes week by week.
Occurs in around 2% of the population and is mostly asymptomatic, although some patients note increased sensitivity to acidic and spicy foods. These periods of sensitivity may occur when patients are stressed or ill. Asymptomatic patients require no treatment.

Areas of slight depapillation of the dorsal surface of the tongue, which are slightly depressed and erythematous surrounded by grey-white areas.
Generalised erythema (redness), desquamation (skin peeling) and oedema of the gingiva usually effecting the whole of the attached gingivae. Desquamative gingivitis is a clinical term describing the appearance. The cause of desquamative gingivitis is most often oral lichen planus, but can also be the clinical appearance of a vesiculobullous condition (fluid filled lesions) such as pemphigoid or pemphigus.
Patients will often experience pain with tooth brushing, leading to plaque-induced gingivitis and periodontitis. However, this condition needs to be recognised separately and the underlying cause diagnosed and treated. Enhanced oral hygiene alone will not resolve desquamative gingivitis and will lead to continued persistence, pain and suffering.

Painful area of erythema of the gingivae extending from the mesial of the upper right central to the gingival margin of the upper right canine. A small erythematous area is also present apical to the upper left lateral incisal gingival margin. These areas were very painful to touch, making toothbrushing very difficult.

Erythema and ulceration across the labial maxillary gingivae extending into the labial sulcus. Very little plaque present.

Erythema with faint striae on almost all the labial gingivae but separate from the free gingival margin that appears normal.

Extensive erythema across the anterior maxillary labial gingivae with areas of ulceration particularly around the upper right canine
Benign increase in the length of the filiform papillae (responsible for giving the tongue its texture and the sensation of touch) on the posterior dorsal aspect of the tongue, resulting in hair-like projection and a coated appearance. This is caused by an increased accumulation of keratin and/or diminished normal desquamation. It may be a result of a change in diet to insufficient coarse foods, often seen in hospitalised very ill patients, or related to salivary hypofunction caused by either systemic medications, Sjogren’s Syndrome or radiotherapy.
The colour of hairy tongue can vary substantially from deep black to white, and is dependent on both the resident bacteria and food debris.

On the posterior aspect of the dorsal surface of the tongue are quite extensive elongated filliform papillae, some of which are very darkly pigmented. These become more pronounced posteriorly. This patient had no symptoms.
Primary herpetic gingivostomatitis
Recurrent herpes labialis (cold sores)
Secondary infection with herpes simplex virus type 1 (HSV-1) that effects the vermillion of the lip with recurring sores following a pattern of slight paraesthesia, redness, appearance of vesicles, superficial ulceration, crusting and eventual healing over a period of 5 to 7 days. HSV-1 resides in the trigeminal ganglion latently after the initial primary infection, primary herpetic gingivostomatitis, that causes a widespread infection with fever, malaise, lethargy and widespread ulceration of the oral mucosa and gingivae over a period of 7 to 10 days. This primary infection mostly occurs in infants, when it is not as severe, but can be seen following oral sex in a seronegative young adult. Recurrent herpes labialis occurs in about 25-30% of individuals and is usually precipitated by concomitant illness, exposure to sunlight or wind and in immunocompromised individuals when it can become severe and prolonged.

Crusting ulcers on the right lower lip at the junction of the vermilion and skin that were previous vesicles that burst several days before this presentation.
Verruca vulgaris
Squamous papilloma
Benign, small isolated outgrowths of the oral mucosa that can have small finger-like projections resulting in a rough cauliflower-like surface. These are caused by non-oncogenic sub-types of human papilloma virus (HPV), usually 1, 6, 11 or 57. Acquired by direct contact or self-inoculation. These growths can be removed if unsightly or interfering with good oral hygiene.
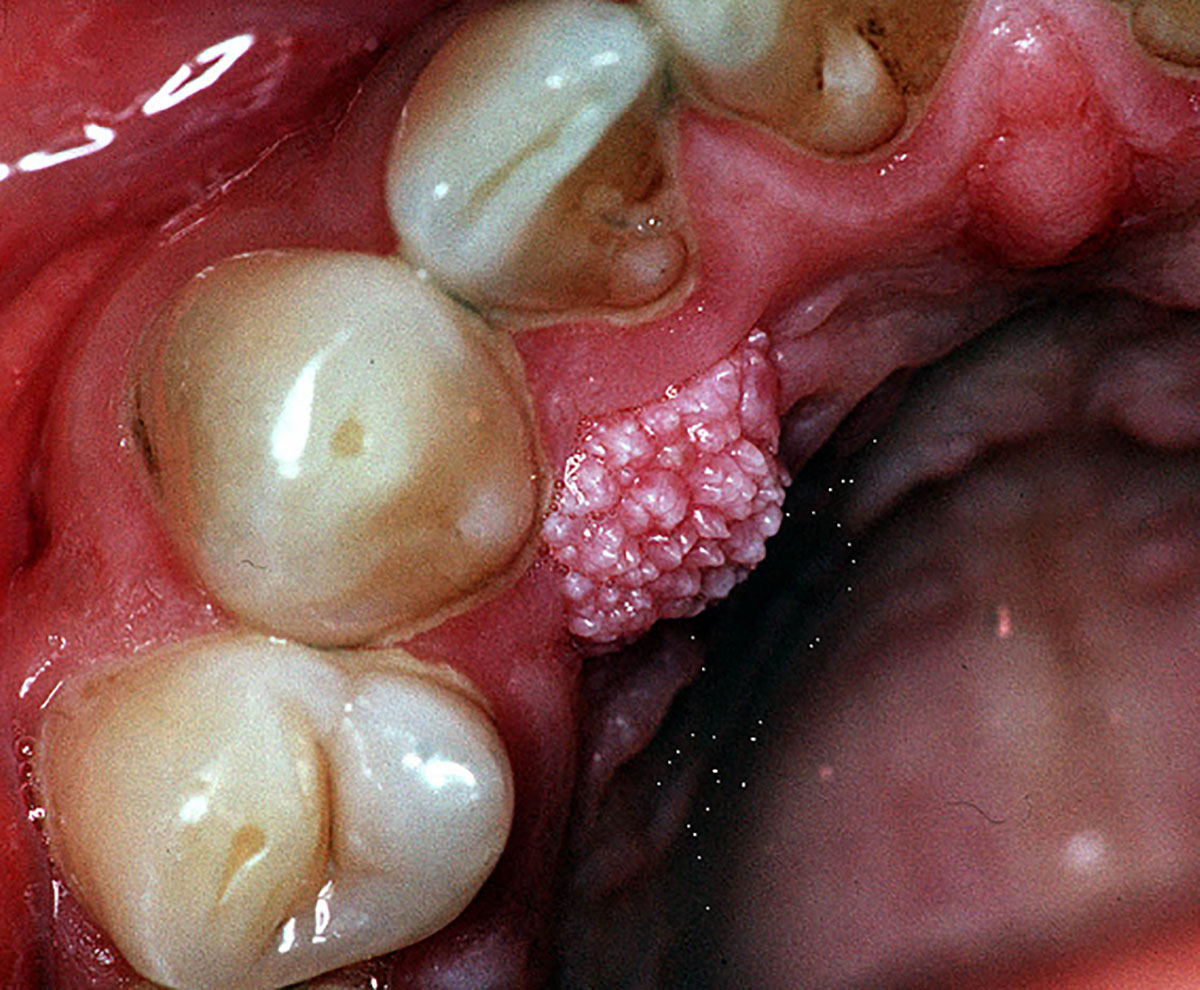
An exophytic mass on the palatal mucosa close to the gingival margin of the upper right canine that has a rough cauliflower-like surface. This was asymptomatic and been present for many years.
Angular chelitis
Fissured erythematous lesions occurring ion one or both corners of the mouth. Thought to be caused by Candida spp. as well as bacteria, usually Staphylococcus aureus. Predisposing factors include anaemia, immune dysfunction or maceration of these areas due to constant presence of saliva. This can occur from a loss of vertical dimension due to old age or poor dentures. Occasionally seen in children, caused by lip licking and biting the corners of the mouth.

Extensive painful erythema on both left and right angles of the mouth.

Left angle of the mouth with erythema and ulceration.
Denture-associated erythematous stomatitis
Erythema (skin redness) of the palate where it meets the surface of a denture. Although an overgrowth of commensal Candida spp. is often present, the principal cause is an ill-fitting denture, poor denture hygiene or nocturnal denture wearing. There is no strong evidence that Candida spp. are the aetiological agents for this condition, so anti-fungal treatment is not warranted. Good denture hygiene with the removal of the biofilm present on the denture surface is adequate, potentially combined with the replacement of an ill-fitting denture.
Pronounced erythema across the whole area of the palate where the fitting surface of an ill-fitting denture contacted in a patient with poor denture hygiene practices.
Pseudomembranous candidosis (oral thrush)
Semi-adherent soft white plaques that can be present on almost all oral mucosal surfaces. When removed, they leave a slightly bleeding, erythematous (red) surface underneath. This frequently occurs in patients who are immunosuppressed, taking long term corticosteroids or have uncontrolled diabetes, as well as the elderly. These lesions are usually asymptomatic unless they extend to the oropharynx and the patient reports a burning sensation in the throat and difficulty in swallowing. Resolution of immunosuppression, if relevant, will resolve these lesions, however topical antifungal medication can aid this process.

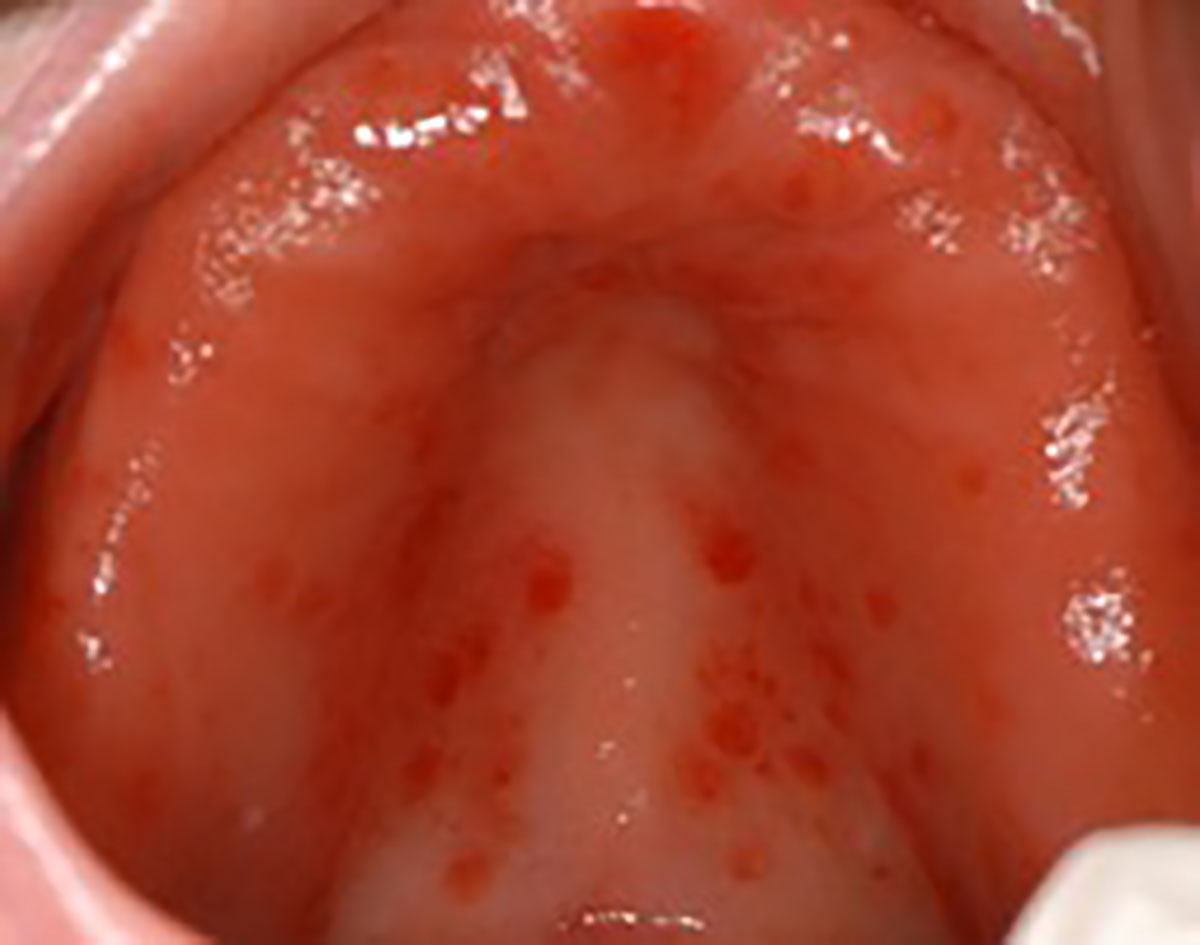
Palatal plaques extending across most of the hard palate with pseudomembranous that could be easily removed leaving the observed erythema. This patient was a poorly controlled asthmatic with heavy use of inhaled corticosteroids.
Soft white plaques that were easily removed to leave an erythematous mucosa on the right buccal mucosa.

Same patient as image above where similar lesions were present of the left buccal mucosa and palate in this immunocompromised patient.
Pemphigus vulgaris
Pemphigus vulgaris is the most common autoimmune intra-epithelial bullous disease that is also potentially life-threatening. It causes blisters on the skin and/or mucosa. Although this is a rare condition, the mouth is affected in about 90% of people and in some patients it will be the only site affected. Accompanying oral lesions are poorly defined, irregular persistent ulcers.

Extensive painful erythema, ulceration and deflated bullae across the soft palate in this patient with pemphigus vulgaris.
Mucous membrane pemphigoid
A rare mucosal autoimmune sub-epithelial blistering disease, with a wide variation in severity: from mild, almost painless oral ulceration, to severe blisters with scarring affecting the mouth, larynx, oesophagus and conjunctiva which can lead to blindness.

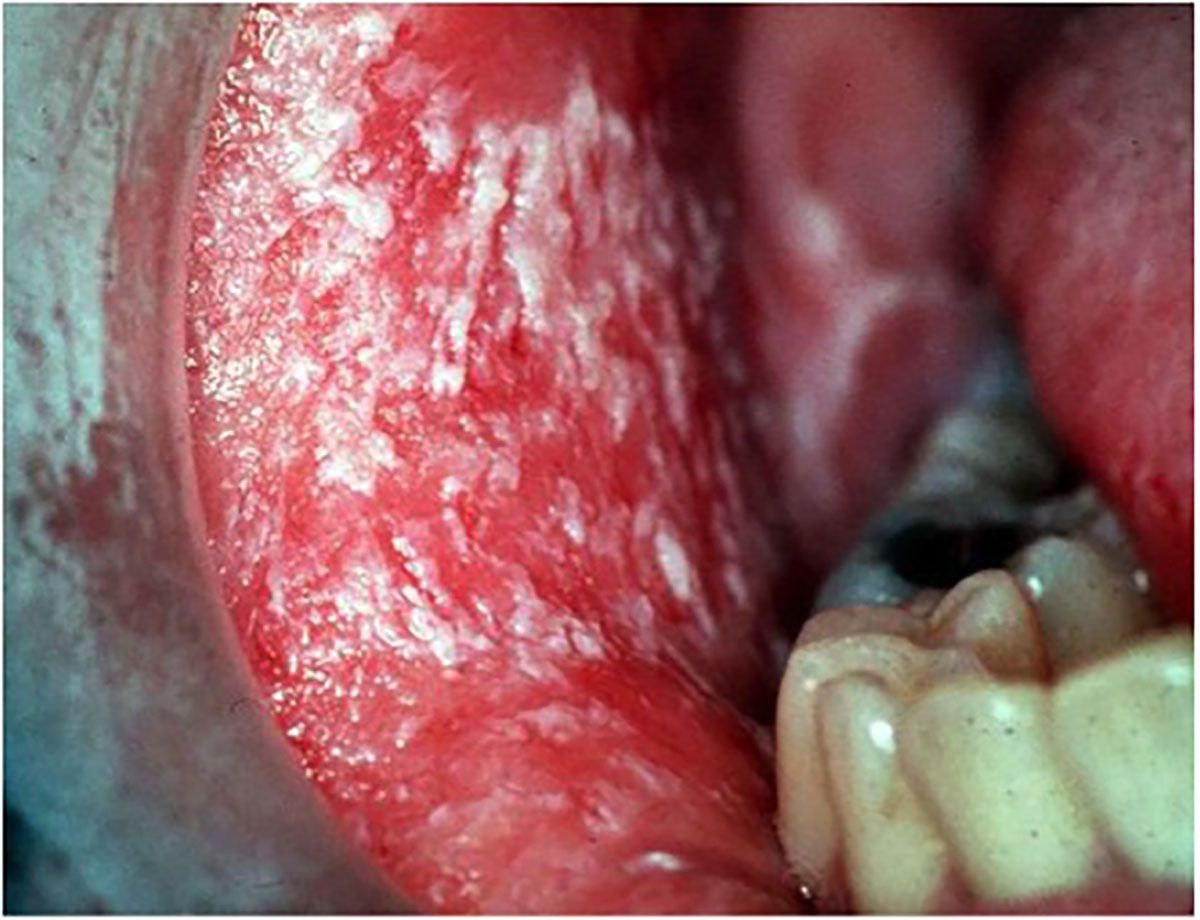
Painful ulceration across the left buccal mucosa surrounded by bright erythema

Deflated bullae that has ulcerated with surrounding erythema on the right lateral margin of the tongue in the same patient as imaged above.