Angular chelitis
Fissured erythematous lesions occurring ion one or both corners of the mouth. Thought to be caused by Candida spp. as well as bacteria, usually Staphylococcus aureus. Predisposing factors include anaemia, immune dysfunction or maceration of these areas due to constant presence of saliva. This can occur from a loss of vertical dimension due to old age or poor dentures. Occasionally seen in children, caused by lip licking and biting the corners of the mouth.

Extensive painful erythema on both left and right angles of the mouth.

Left angle of the mouth with erythema and ulceration.
Denture-associated erythematous stomatitis
Erythema (skin redness) of the palate where it meets the surface of a denture. Although an overgrowth of commensal Candida spp. is often present, the principal cause is an ill-fitting denture, poor denture hygiene or nocturnal denture wearing. There is no strong evidence that Candida spp. are the aetiological agents for this condition, so anti-fungal treatment is not warranted. Good denture hygiene with the removal of the biofilm present on the denture surface is adequate, potentially combined with the replacement of an ill-fitting denture.
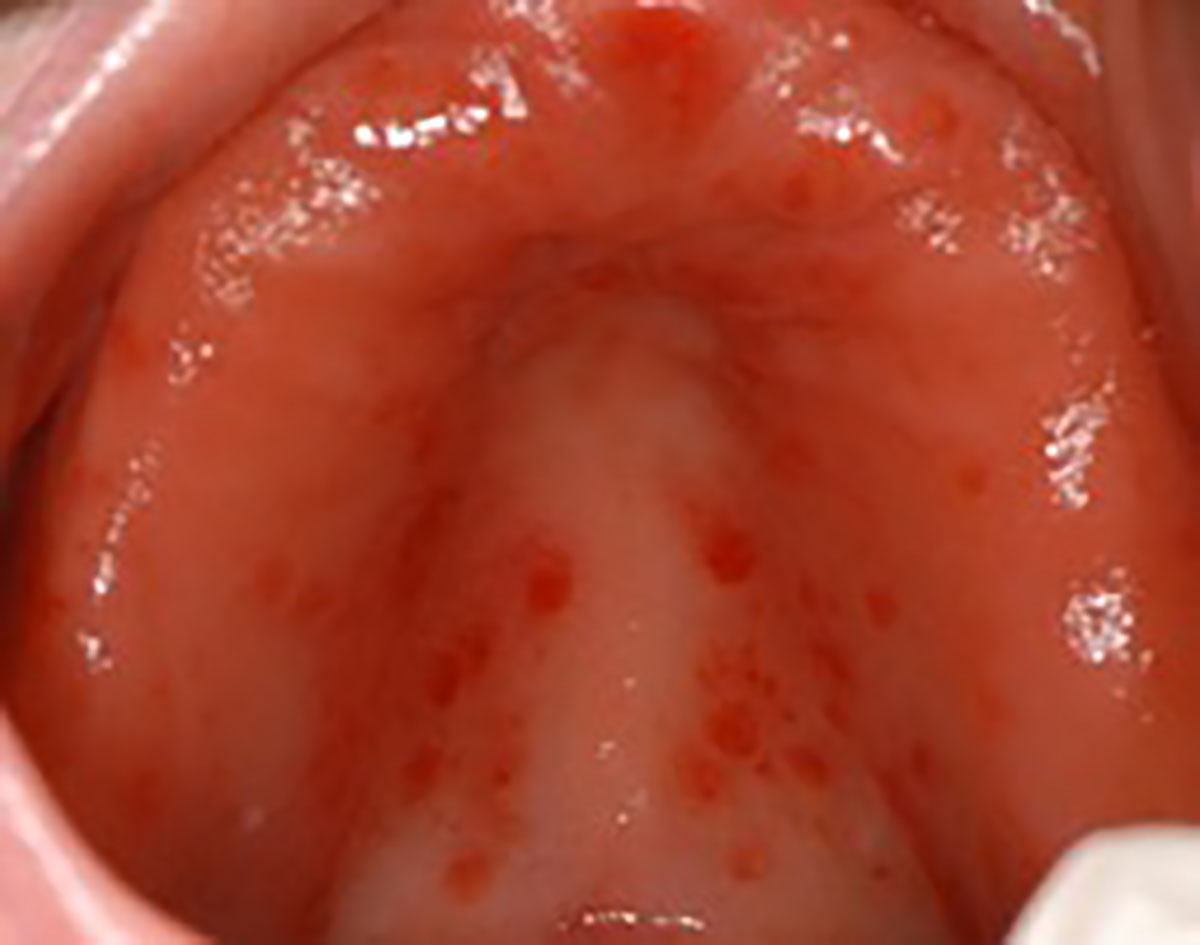
Pronounced erythema across the whole area of the palate where the fitting surface of an ill-fitting denture contacted in a patient with poor denture hygiene practices.
Pseudomembranous candidosis (oral thrush)
Semi-adherent soft white plaques that can be present on almost all oral mucosal surfaces. When removed, they leave a slightly bleeding, erythematous (red) surface underneath. This frequently occurs in patients who are immunosuppressed, taking long term corticosteroids or have uncontrolled diabetes, as well as the elderly. These lesions are usually asymptomatic unless they extend to the oropharynx and the patient reports a burning sensation in the throat and difficulty in swallowing. Resolution of immunosuppression, if relevant, will resolve these lesions, however topical antifungal medication can aid this process.

Palatal plaques extending across most of the hard palate with pseudomembranous that could be easily removed leaving the observed erythema. This patient was a poorly controlled asthmatic with heavy use of inhaled corticosteroids.
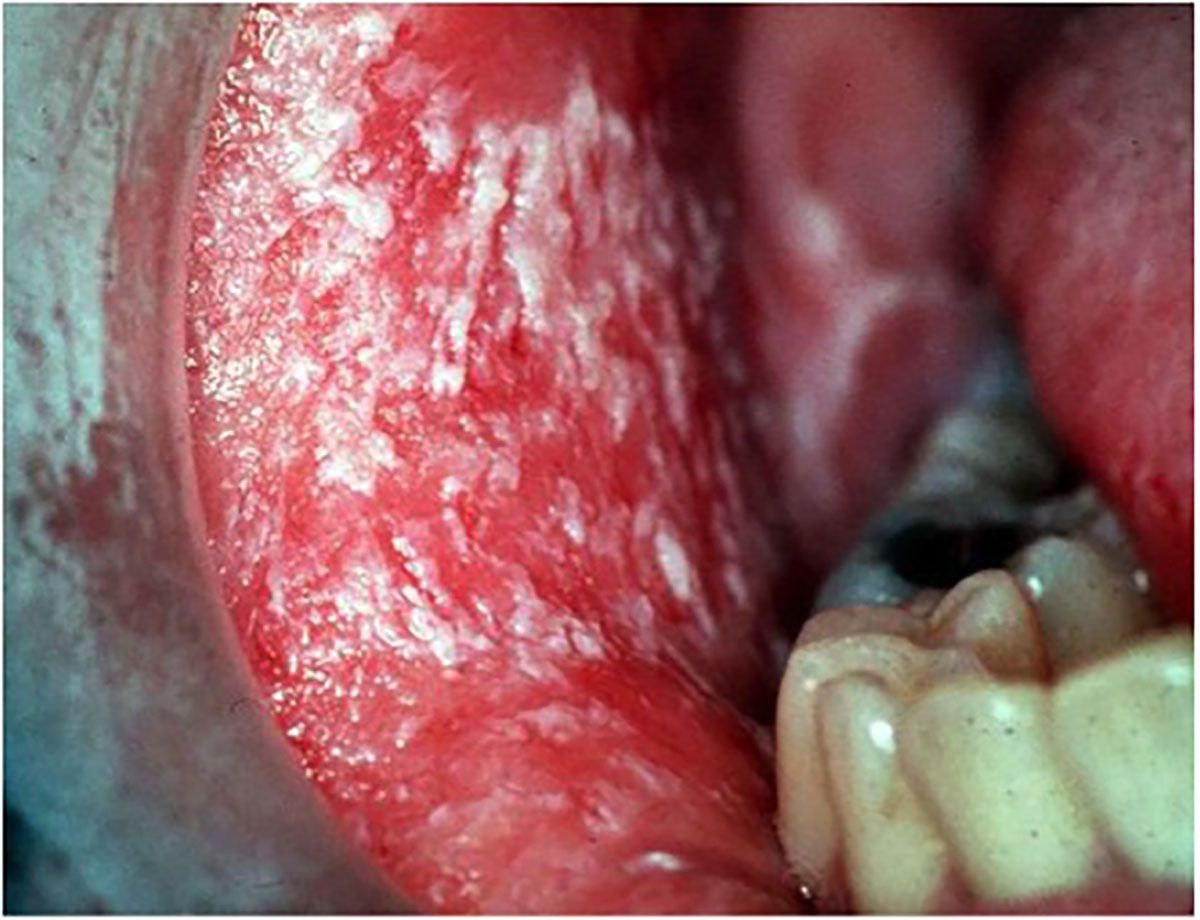
Soft white plaques that were easily removed to leave an erythematous mucosa on the right buccal mucosa.

Same patient as image above where similar lesions were present of the left buccal mucosa and palate in this immunocompromised patient.